My name is Mary Schaff. I am a grandmother, a mother, a widow and an advocate. My late husband John and I shared a deeply personal and troubling relationship with sleep apnea. It is my hope that in telling our story, others have the possibility of a very different outcome.


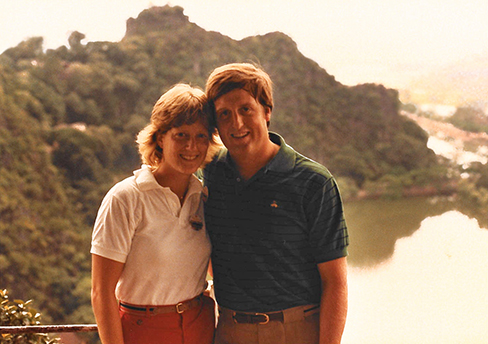





John & Mary - Our Story
More than Just Snoring
My husband John snored much of his adult life. While it increased in frequency and intensity in his early 40s, he dismissed it as a minor annoyance. Even after he began experiencing side effects from failing to achieve healthy deep sleep, he was quick to brush off my concerns and refused to acknowledge something was wrong, often saying “It’s just snoring” and “It’s nothing to worry about.” At this time, neither of us was aware of sleep apnea.
We led an active life, with regular exercise and frequent travel. However, John’s sleep problems persisted over the next decade and began to negatively impact our daily activities. These included nodding off in church, falling asleep watching TV and in the office, and once even starting to doze off at the wheel.
John did see his doctor regularly, but nothing stood out to his physician as a warning. Routine blood and cholesterol tests were normal, everything checked out fine. The doctor did recommend John lose some weight. John, a lifelong athlete, unsuccessfully sought to address his weight with diet and exercise. Sleep was not a part of the conversation.
I encouraged John to have a sleep test to get to the bottom of his daytime tiredness, but he held out, citing reports from friends that the in-clinic test was a “horrible and uncomfortable” experience. I had a nagging suspicion that something was wrong, and I believe John did too, as he eventually ordered a CPAP machine. Like many others, John found the initial CPAP mask uncomfortable and quit using it after only three nights. Neither of us realized the device needed to be individually pressurized by a technician to properly work.
It was a new internist who had experience with sleep disorders who finally connected the dots and suspected John suffered from sleep apnea. The years of interrupted sleep and arrested breathing slowed his metabolism to a standstill because his body had been severely deprived of oxygen. The doctor’s explanation was clear and John agreed to a sleep test. This felt like true progress.
Sadly, John died of cardiac arrest two days before the test to determine the course of treatment. The lack of oxygen to his organs over time had unknowingly damaged his heart. Sleep apnea was listed on his death certificate as a contributing cause of John’s death. He was 57 years old.
Mary’s Story
From Tragedy to Advocacy
Immediately following John’s death, I began researching, looking further into why the link between sleep apnea and other diseases and conditions is so often overlooked. Experts calculate one in three adult Americans is affected by obstructive sleep apnea in the United States alone. However, the vast majority is either unaware or unclear that this common and highly treatable disease relates to them. During my research I was amazed to discover that in several years of medical school, many students receive less than five hours of education in sleep-related disorders.
My goal is to help generate conversations that bring awareness to this potentially life-threatening condition – conversations within families, and with friends and physicians. It’s as simple as starting with “How are you sleeping?” With early detection and proper treatment, people can go on to live full lives with sleep apnea.
In my quest to learn more about sleep apnea, I’ve become acquainted with leading sleep expert and neurologist Dr. Nancy Foldvary-Schaefer, DO, MS, director of the Sleep Disorders Center at the Cleveland Clinic. Cleveland Clinic’s Sleep Disorders Center was among the first in the nation dedicated to the diagnosis and treatment of sleep disorders in those of all ages.
The efforts of Cleveland Clinic’s Sleep Disorders Center dovetail with my interest in education and awareness of sleep apnea. The center is actively engaged in the continuing medical education on sleep disorders for physicians, creating greater awareness among primary healthcare providers. Additionally, the Sleep Disorders Center developed a mobile sleep app designed to help screen for sleep apnea - Sleep by Cleveland. The free app encourages individuals to seek necessary treatment and provide a means for patients to stay connected with their physicians and exchange, in real-time, critical information.
I have had the pleasure of speaking at various forums about John’s and my story, and will continue to seek opportunities to do so. As my family and friends can attest, I take every opportunity to have these conversations, in my personal life and publicly.
Nothing can lessen the magnitude of my loss. I cannot bring John back. However, it is my hope that my story – our story – and the information shared here can inspire you or your loved ones to start the conversation and take action before it may be too late.